The Centers for Medicare & Medicaid Services (CMS) released the 2018 Physician Fee Schedule about two weeks ago and there is at least one nugget in there that should speed the adoption of remote patient monitoring. In fact, the news is even better, but I’m getting ahead of myself. First, let’s examine the broader context of what adoption of remote monitoring will mean for healthcare delivery and the amazing story of how we got here.
Why it matters
By 2050, 16% of the world’s population will be over 65, more than double the number under five years old. Inevitably, older people require more healthcare resources and caregiving. The math is too stark to ignore: we’re running out of young people to care for our elders if we continue to offer only one-to-one, face-to-face care as an option. If you want to learn more about this conundrum, it is covered in some detail in my new book, The New Mobile Age: How Technology Will Extend the Healthspan and Optimize the Lifespan.
Remote monitoring is critical to move us from one-to-one models of care delivery to one-to-many. Other services have done this, and we need to catch up. At Partners Connected Health, in collaboration with colleagues in our delivery system, we have shown, more than once, that home monitoring of patients with congestive heart failure leads to lower hospitalization rates and improved mortality. Others have shown this too. In this type of remote monitoring system, the nurse to patient ratio is about 1:100. That’s what I mean by one-to-many.

Yet, to date, most telehealth has been delivered via videoconferencing between patients and doctors. These interactions have improved access, but still rely on that one-to-one model. Stated another way, video communication breaks the ‘place’ barrier but remote monitoring is both time and place independent — a challenge for healthcare providers who are used to thinking that healthcare should be rendered in the doctor’s office.
A survey, published by the American Medical Association (AMA) in 2016, succinctly outlined the barriers to digital health adoption among physicians:
* Need for evidence
* Reimbursement
* Liability coverage
* Workflow/EMR integration
These insights have driven AMA’s digital health strategy since. For the last year, I’ve had the privilege of working with them on several aspects of this, including co-chairing their Digital Medicine Payment Advisory Group (DMPAG), which has focused on reimbursement for digital medicine, including remote monitoring.
The specific news
In 2004, I took my kids to the Lemony Snicket movie, “A Series of Unfortunate Events”. The story on Medicare reimbursement for remote monitoring is just the opposite: many dedicated people working, sometimes in coordination and sometimes not, at the right place and right time in history, culminating in a series of fortunate events.
Here are the specifics of what we learned when the 2018 Physician Fee Schedule was released on November 3:
CMS has decided to unbundle and activate CPT code 99091 (collection and interpretation of physiologic data). CMS has stated that this is an interim step until the Agency considers new CPT codes and valuation recommendations.
CMS stated in the rule that the Agency “look[s] forward to forthcoming coding changes through the CPT process that [they] anticipate will better describe the role of remote patient monitoring in contemporary practice and potentially mitigate the need for the additional billing requirements associated with these [99091] services.”
This is an amazing announcement since, for decades, Medicare had turned a deaf ear to most forms of telehealth and any discussion of remote monitoring was relegated to the depths of despair.
How we got here
When providers perform a task related to your care, they document the work using a common procedure coding system which includes a number of codesets such as the one maintained by the Current Procedural Terminology (CPT) Editorial Panel. In most cases, these codes are used to electronically bill your insurer, who then pays the provider according to a contracted fee schedule. The CPT Editorial Panel has been around for decades and though the members, comprised of a cross-section of healthcare stakeholders including insurers, are appointed by the AMA Board of Trustees, the Panel’s decision-making is independent of the AMA.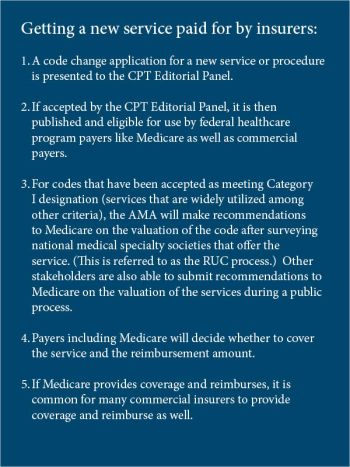
The code change application process can occur in a relatively rapid period of time—a matter of months from the date the application is submitted to the date it is considered by the CPT Editorial Panel. However, the Medicare program’s process for considering recommendations for valuation and coverage (through the rulemaking process) can be lengthy because such decisions are made on an annual basis. Hence, the Medicare process takes years and a code can be derailed at any point. Medicare can choose not to pay for a code and they can also choose to ‘bundle’ the code, if the work related to that code is already covered in their reimbursement of other services.
The classic example is the code that reimburses doctors for telephone calls with a patient. Insurers don’t pay because Medicare decided that telephone follow up is included in reimbursement for an office visit. It is important to note that commercial payers can utilize the codes as soon as they are publicly posted by the CPT Editorial Panel and are not required to follow the Medicare process for valuation and coverage.
The importance of the new fee schedule is this: although CPT code 99091 has existed for years, it was bundled. By simply unbundling this code, CMS opened the door for remote monitoring reimbursement. And, because the code exists, it already has an assigned monetary value, so as of January 2018, providers can start to provide remote patient monitoring services and actually receive reimbursement.
This breakthrough is not happenstance. It is the result of two phenomena. One is the dogged pursuit of a handful of individuals who see the mounting challenges of caring for an aging population, and who are passionate that we have to get there for the sake of better patient care. These folks have been lobbying the government for years, and despite countless setbacks, have continued the quest. The second phenomena was the appointment of a new CMS chief, the consequence of a new administration in Washington. Whatever you think of our current administration, it is a fact that they are more telehealth friendly than any in history.
Now, getting back to the work of the AMA’s DMPAG, we recently put forward three code change applications to the CPT Editorial Panel, including two related to remote monitoring. This too was not a random event. The AMA wisely populated this advisory group with half digital health experts/practitioners and half CPT/RUC experts. We’ve worked well together and the AMA deserves enormous credit for their wisdom and support.
So it was with great thought and preparation – and no guarantee of success – that we presented these proposed new codes in September and the CPT Editorial Panel, which acts independent of the AMA, approved them so our success was not guaranteed. We felt a sense of victory, but also vulnerability, as we don’t have particular influence over the RUC valuation and even less over whether CMS will reimburse for the new codes. At the time, I reminded our DMPAG team that the apt sports analogy for this success was a first down rather than a touchdown.
This changed significantly with the November 3 announcement and the specific wording that CMS looks forward to new codes from the CPT process.
The wheels could still fall off the wagon. We can’t let up in our quest.
It must also be pointed out that there are other adoption barriers clearly identified in the 2016 AMA survey. Reimbursement, however, is a big one. With reimbursement comes enthusiasm from EMR vendors to improve workflows and processes. As the CPT Editorial Panel only approves codes that have sufficient evidence, and though some will say there is never enough evidence, the case for remote monitoring is a strong one. And, as we improve workflows, that should also help mitigate liability concerns.

The future is bright for remote monitoring, all of a sudden. But it has taken us years of work and ‘a series of fortunate events’ to get there. I’ve been privileged to be part of an amazing team that the AMA gathered, and fortunate to benefit from the hard work of others to move thinking on this topic at CMS.
Our patients of all ages will benefit and, importantly, we can achieve a one-to-many delivery model in time to care for the oncoming ‘silver tsunami’ of our aging population.
Wanna share this post
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on Skype (Opens in new window)
